Trends, gaps, and community implications
Overview:
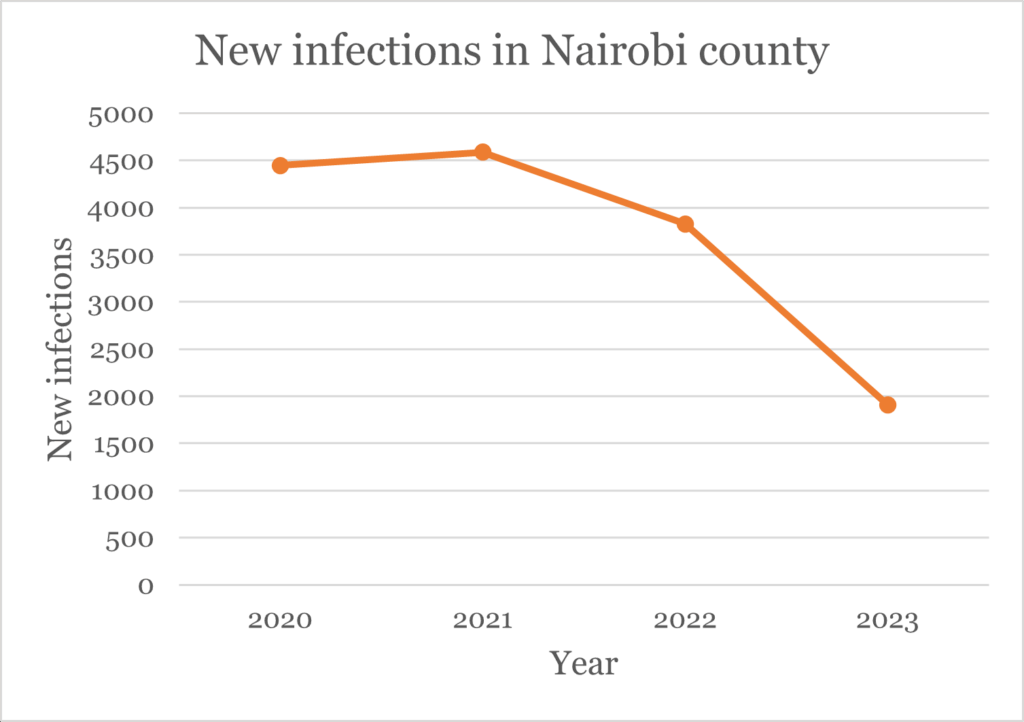
In a recent stakeholders meeting, on 6 August, members noted a decrease in HIV cases since 2021. KCEI data specialists conducted an analysis of these findings to identify why.
Data is a vital tool for guiding decisions and ensuring effective resource allocation. This report analyzes HIV Testing Services (HTS) trends using data from National AIDS and STI’s Control Programme (NASCOP) (2020–2024) and demographic insights from the Kenya National Bureau of Statistics (KNBS).
It focuses on Kamukunji Sub-County in Nairobi, examining the relationship between population share and HTS uptake. The aim is to highlight gaps, contextual drivers, and offer evidence-based recommendations to strengthen HIV response in one of Nairobi’s most dense and vulnerable communities.
Background and context
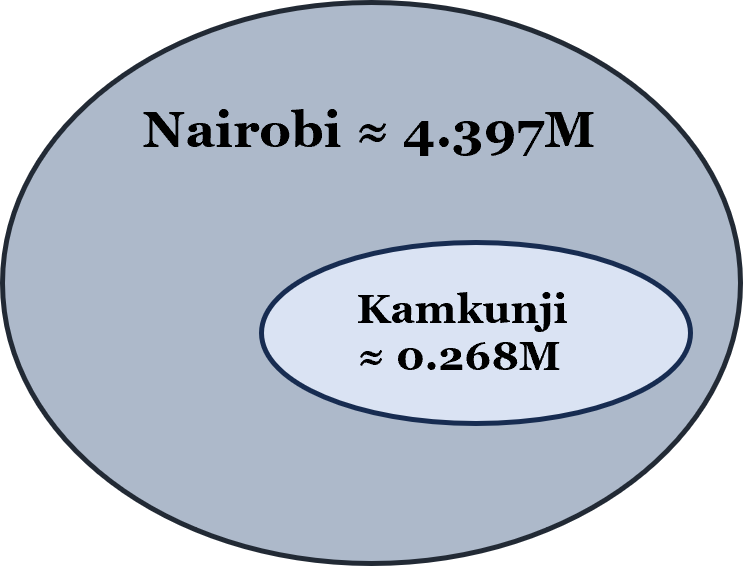
According to the 2019 census, Nairobi accounts for 9.2% of Kenya’s population with approximately 4.397 million residents. Within the county, Kamukunji Constituency represented 6.1% of Nairobi’s population, about 268,000 people, includes Majengo slum.
Majengo and similar informal settlements are marked by poverty, overcrowding, and limited access to healthcare.
Despite a steady decline in new HIV infections in recent years, Nairobi County continues to record the highest number of new cases nationally. Kamukunji Constituency, given its demographic weight and socio-economic vulnerabilities, remains particularly at risk. These dynamics sustain a disproportionately high vulnerability to HIV transmission, posing a significant public health challenge that calls for targeted interventions.
HIV Testing trends between 2020 to 2024:
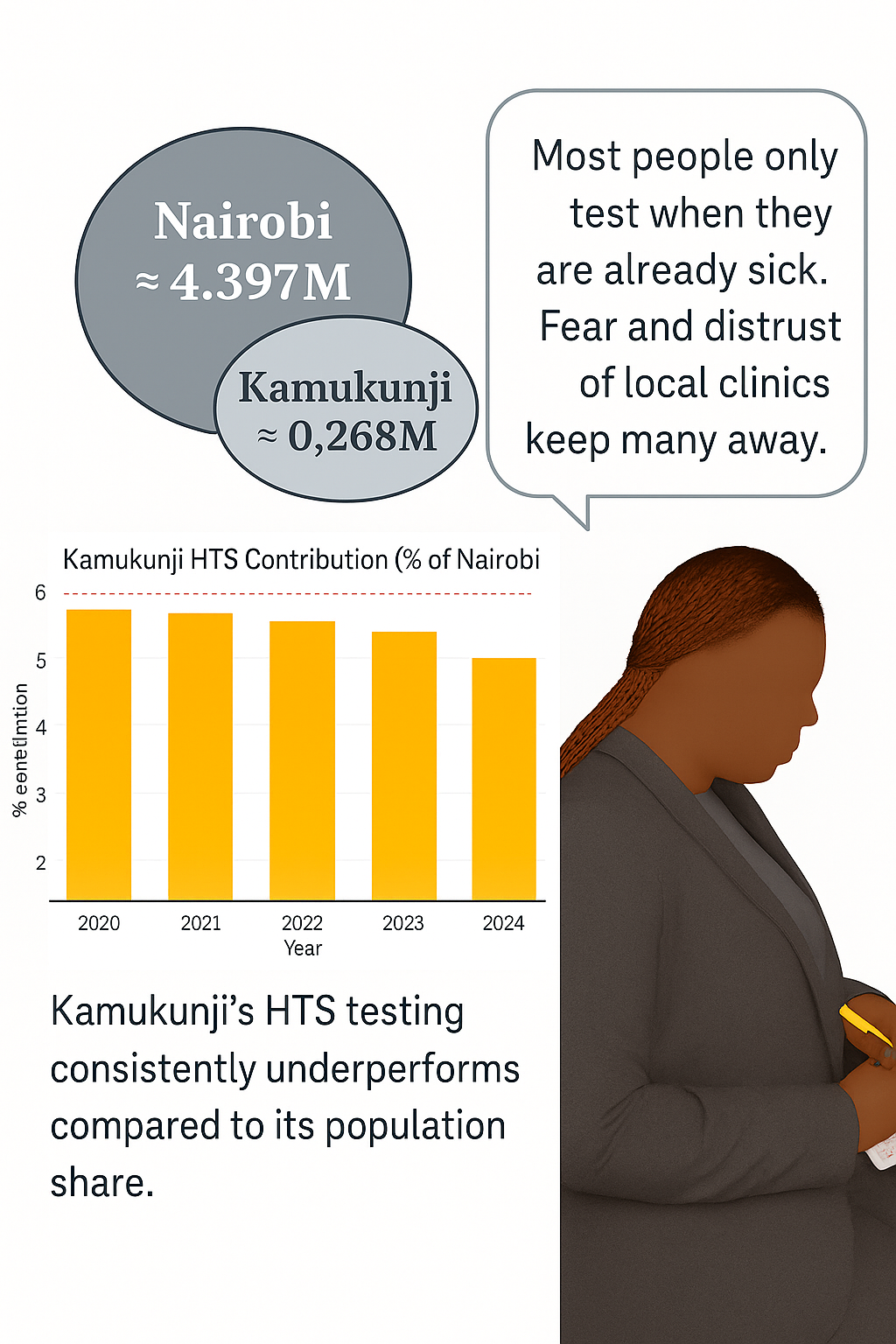
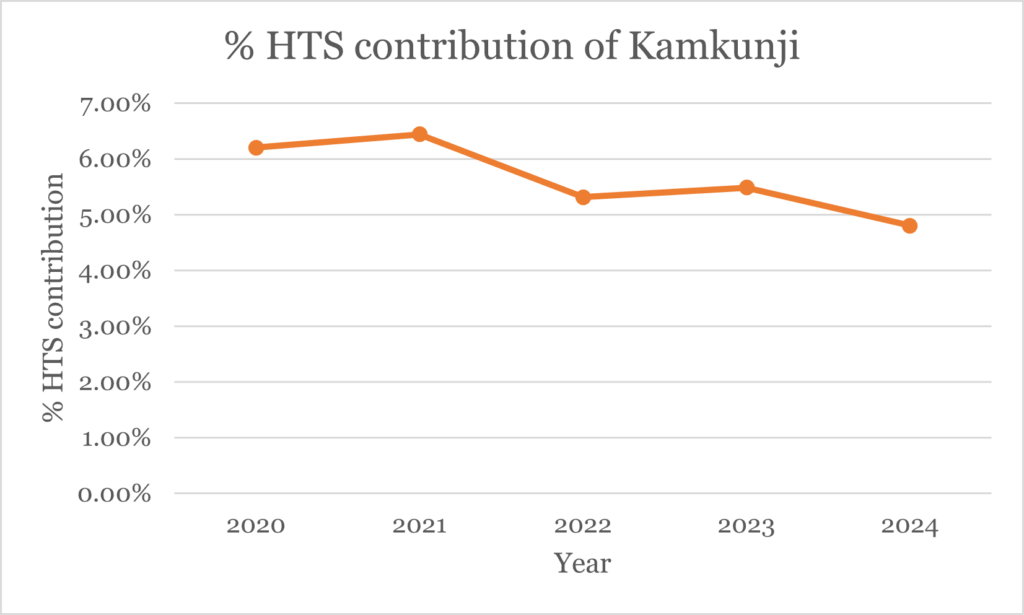
Over five years, Nairobi County recorded an average of 4,730 HIV tests annually, while Kamukunji averaged just 266 tests—about 5.62% of Nairobi's total. This is slightly below its population share of 6.1%, raising concerns about under-testing.
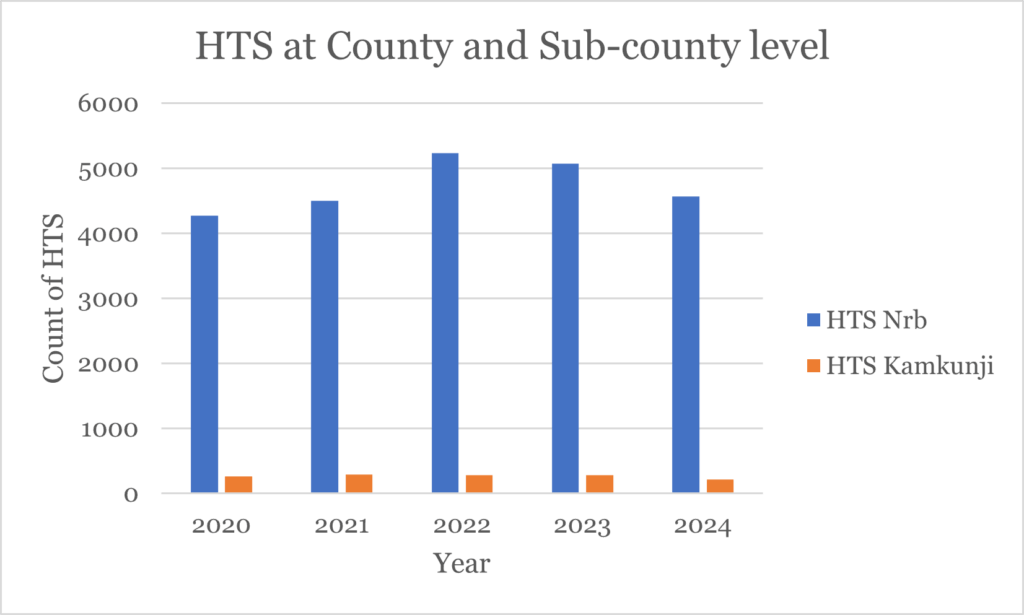
Although population size does not always translate directly into proportional testing contribution, testing has declined since 2022, suggesting challenges in awareness, access, or service delivery.
Limitations of available data:
This report currently lacks gender, age, and key population disaggregation. Disaggregated data is essential to understanding HIV vulnerability in groups such as adolescent girls, sex workers, Men having Sex with Men (MSM), and people with disabilities.
Additionally, no data on HIV positivity yield or linkage to ART (antiretroviral therapy) is presented, which limits our understanding of outcomes after testing.
Barriers to testing in Kamukunji:
Despite having over 55 facilities offering HTS, testing uptake remains low. Contributing factors include:
- HIV-related stigma
- Limited community-level awareness campaigns
- Fear of discrimination or breach of confidentiality
- Under-resourced health workers and unwelcoming facilities
- Low prioritisation of routine testing, especially among men and youth
Community speaks:
A youth leader from Majengo noted: “People don’t go to test unless they are already sick. There’s fear, and people don’t trust the clinics near them.”
This highlights the emotional and social dimensions behind low HTS uptake.
What the data is telling us:
- Testing levels do not align with Kamukunji’s population size, suggesting potential under-diagnosis.
- Reduced testing since 2022 may increase undetected transmission risks.
- Low uptake undermines early HIV diagnosis and timely ART initiation.
- Under-testing could weaken Nairobi's HIV reduction goals.
What we need to do:
- Conduct community sensitisation through trusted local voices and peer educators.
- Introduce mobile and school-based HIV testing drives.
- Integrate HTS into other community services (e.g., GBV support, mental health).
- Provide incentives for HTS among hard-to-reach groups, especially youth and men.
- Strengthen training and support for facility-based health workers.
- Regularly disaggregate HTS data by gender, age, and key populations to improve targeting.
Way forward:
Kamukunji’s HTS data highlights a pressing need for targeted, community-centered HIV interventions. Addressing social stigma, improving access, and incorporating community voices into outreach will be key to reversing current trends. With stronger political will, investment, and monitoring, Kamukunji can be a model constituency in helping Nairobi and Kenya meet HIV response goals.
By Akelle Waguma| Media and Communication Strategist, and Patrick Ouma Ombok| Data scientist, Risk and Compliance Officer.

